How AI Is Revolutionising Allied Health Service Delivery
The breadth of innovation in AI that currently exists for allied health is already quite breath-taking. Much of the clinical innovation is in the physical therapies—particularly rehabilitation—but there is a growing suite of sophisticated tools that provide mental health support, education and monitoring. Most of these tools are available remotely, reducing patient and practitioner travel while increasing the accessibility to scarce services and the potential to improve clinical efficiencies.
AI is also increasingly valuable to support service efficiency and innovation. Examples include automated scheduling systems that send reminders to help reduce the rate of appointment non-attendance; improved clinical documentation and recording; searching of health records to find relevant information to reduce duplication and inefficiency in diagnosis and testing; and use in triage and assessment.
There are also some examples of the use of AI, and more specifically, technologically-based tools to support team collaboration. Many of these tools are reasonably well-integrated into practice now, and perhaps require tweaking to improve their effectiveness in brokering teamwork.
Will this change the way that the allied health professions work? Absolutely and without doubt. Just a quick skim of the applications of AI below shows that this is a rapidly evolving field with implications for every area of allied health practice from training and education to service delivery and practice/service management.
This article explores the transformative potential of AI for the allied health professions. From virtual reality therapy to intelligent diagnostic tools, a range of innovative solutions are revolutionising patient care and empowering allied health professionals to substantially change the way they work and to increase their impact and service reach.
How can AI benefit the work of the allied health professions?
AI can significantly benefit the work of allied health professionals in various ways, improving efficiency, accuracy, and overall patient and client care. Some examples include:
Enhanced diagnostics and decision support: AI algorithms can analyse complex medical data, including medical imaging, lab results, and electronic health records to assist in diagnosis, treatment planning, and predicting patient outcomes.
Workflow optimisation: AI can streamline administrative tasks such as appointment scheduling, billing, and inventory management, allowing professionals to spend more time on direct patient care.
Telemedicine and remote monitoring: AI-powered telemedicine platforms can facilitate remote consultations, allowing patients to receive care from allied health professionals without the need for in-person visits. Additionally, AI can help remotely monitor patients’ conditions, alerting professionals to any concerning changes.
Personalised treatment plans: AI can analyse patients’ medical data to identify the most effective treatment options, tailoring care to each individual’s unique needs and improving outcomes.
Patient education and engagement: AI-driven tools can help patients better understand patient conditions and treatment options, promoting adherence to care plans and enhancing patient-provider communication.
Collaboration and communication: AI can enable better collaboration among allied health professionals, promoting effective communication and knowledge sharing, ultimately leading to better patient care.
Training and education: AI-powered simulations and virtual reality environments can help train allied health professionals, enhancing their skills and knowledge in a controlled, risk-free setting.
Research and development: AI can analyse large datasets to identify patterns and correlations, driving new discoveries and innovations in the field of allied health.
AI has the potential to revolutionise the work of the allied health professions, improving the quality of care and making healthcare more accessible and personalised for patients. However, it is crucial to ensure that AI is implemented ethically, with due consideration given to privacy and security concerns, as well as the need for human oversight and collaboration.
Each of the points above is expanded in more detail below.
Enhanced support for diagnostics and decision-making
Increasingly, machine learning and AI applications are being deployed in allied health and medicine to analyse large datasets to identify patterns for early and accurate disease diagnosis, improving treatment effectiveness. AI excels in areas like radiology, for example, interpreting MRIs, X-rays, and CT scans with high accuracy and speed.
Patient and client care are being personalised via AI analysis of medical histories, genetics, and lifestyles to predict health risks and suggest individualised treatment plans.
Additionally, predictive analytics can anticipate public health trends, aiding in managing and containing infectious diseases. In rehabilitation and chronic disease management, AI monitors patient progress through wearable devices, adjusting treatment plans in real-time for optimal recovery.
There are several examples of AI-based decision-making support systems being deployed by the allied health professions.
Physiotherapy and rehabilitation: AI-driven tools such as BioGears and Sword Health provide personalised exercise programs and real-time feedback on patients’ performance, helping physiotherapists to optimise treatment plans and track progress more effectively. Such applications can assist physiotherapists by analysing patient data, such as movement patterns and medical history, to identify patterns and anomalies.
Speech therapy: Applications like Constant Therapy and TalkPath Therapy use AI algorithms to assess patients’ speech and language abilities by analysing speech patterns, language development, and voice data to tailor therapy programs accordingly.
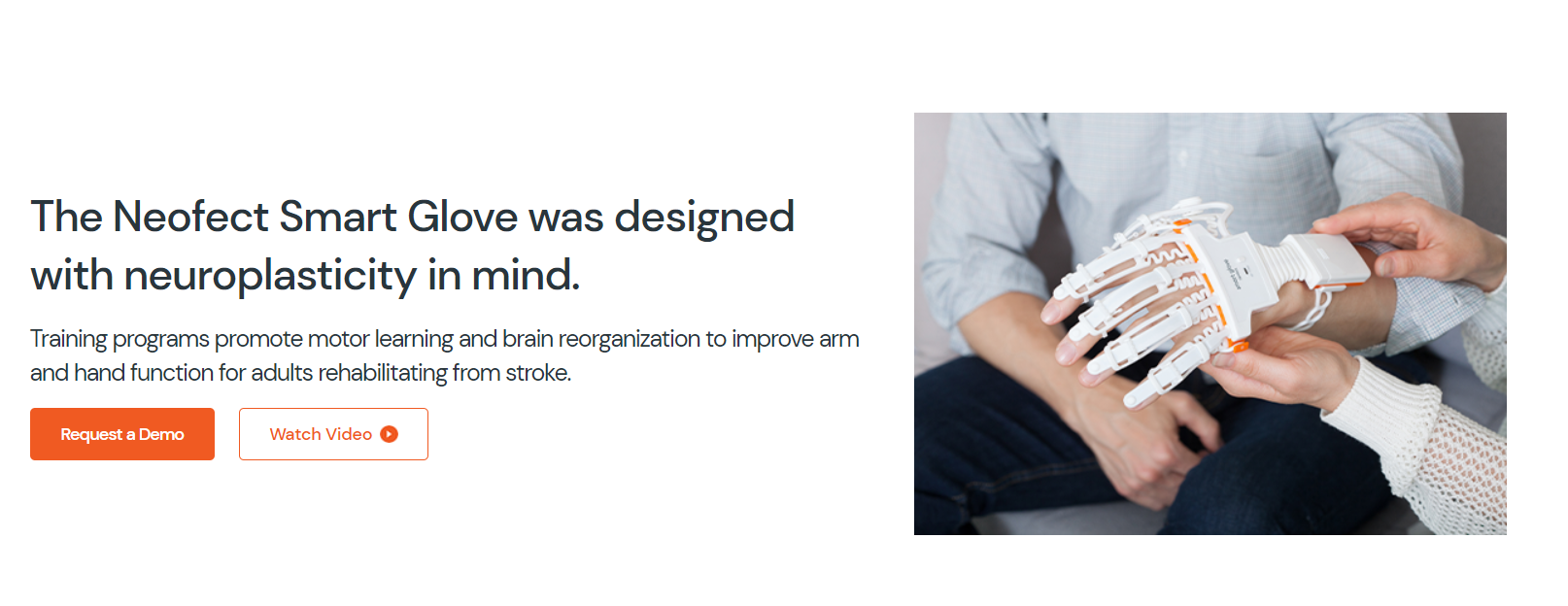
Occupational therapy: Platforms such as Neofect Smart Rehab and FlintRehab use machine learning—and in the case of FlintRehab, gamification—to develop customised rehabilitation programs for patients with neurological and musculoskeletal disorders, supporting occupational therapists and others to deliver personalised care.
Nutrition and dietetics: Nutrino, PlateJoy, and EatLove analyse users’ dietary preferences, nutritional needs, and health goals to generate personalised meal plans and recommendations, assisting dietitians in providing tailored advice and guidance.
Mental health and counselling: Chatbots and virtual therapists such as Woebot and Tess support mental health professionals by providing users with evidence-based techniques and resources for managing stress, anxiety, and depression, supplementing traditional therapy sessions.
Audiology: Decision-making support systems like SHOEBOX Audiometry and OtoNexus can assist audiologists in diagnosing and treating hearing disorders, analysing test results, and recommending appropriate interventions.
Optimised workflow in practice/service management and delivery
Machine learning and AI are starting to transform workflow optimisation in allied health settings via automated resource allocation and the simplifying of administrative tasks.
By automating data management, these technologies significantly reduce the time spent on analysing patient records and diagnostic information, allowing healthcare providers more time for direct patient care. Electronic health record (EHR) systems such as those provided by Cerner, Epic, CareRight and Veradigm, can help health professionals to access relevant patient information, predict potential health risks, and suggest appropriate interventions.
Practice and clinic management can potentially be improved through the optimisation of appointment scheduling and predicting patient and client no-shows. Zocdoc and 10to8 are examples of platforms that use AI and machine learning to automate appointment scheduling and reminders.
AI is increasingly being adopted to simplify administrative tasks in healthcare settings, automating billing, coding, and claims processing. A number of well-known platforms, including 3M, Xero and MYOB, are promoting AI functionality. This not only streamlines administrative processes but also accelerates reimbursement procedures.
Triage and patient flow are additional aspects of allied health clinical workflow experiencing the impact of machine learning and AI. AI-driven assistants like Sensely’s Molly and Microsoft’s Azure Health Bot are claiming to triage patient inquiries, answer common questions, and route more complex issues to the appropriate professionals.
Aidoc and Zebra Medical Vision state the ability to identify urgent cases by analysing medical images and other clinical data, enabling healthcare professionals to prioritise high-risk patients and expedite care. And analytics platforms like Qventus and LeanTaaS suggest a functionality of predicting patient/client demand.
Remote monitoring and personalised treatment plans
AI is playing an increasingly important role in telemedicine and remote monitoring, analysing data from wearables and electronic health records. It identifies health trends and risks, allowing health professionals to tailor treatments to individual needs and intervene promptly; AI-driven remote monitoring solutions such as Biofourmis, for example, can track patients’ vital signs, activity levels, and other health parameters, alerting AHPs to concerning changes and facilitating timely interventions.
Physiotherapy and rehabilitation: An increasing number of tele-rehabilitation platforms (such as Physitrack and TheraNow) are incorporating AI to create personalised exercise programs, monitor patients’ progress remotely, and provide real-time feedback on their performance, enabling physiotherapists to offer effective remote care. The AI offers guidance on exercise routines typically supervised in a clinic, potentially beneficial for patients in remote locations or with limited access to health professionals due to work obligations or a busy lifestyle.
Mental health and counselling: BetterHelp and Talkspace are theletherapy platforms that use AI algorithms to match patients with suitable mental health professionals based on their needs and preferences. Additionally, chatbots built on emotion AI such as Woebot increasingly provide supplementary support by offering evidence-based therapeutic techniques remotely.
It remains to be seen whether AI has a role to play in a sector as nuanced, personal, and private as psychological counselling—while AI’s practical presence in mental health is undeniable, and growing, it continues to be a source of controversy.
Privacy and lack of transparency around use of therapy session data is a contentious issue, with data mining of client sessions being used to train proprietary AI. Further innovations, such as an algorithmic response triggered by suicidal ideation keywords and phraseology, is only possible through surveillance and retention of therapy sessions and chat logs, far exceeding the privacy expectations between human therapist and client.
The effectiveness of AI to match clients to telehealth therapists depends on the quality of information the client is able to provide when they sign up for the service, and the quantity of therapists available.
A licensed therapist who signed up for Talkspace found the initial consult—which the AI would base therapist selection on—lacking: “The questions were somewhat vague, and I had to choose from options on a drop-down menu, which I had trouble answering because I wanted to be able to elaborate on my responses. Questions included whether I had been in therapy before, if and when I have ever been hospitalized for my mental health, and if and when I have ever experienced suicidal thoughts. For example, the suicidal ideation question allowed me to select “Never,” “More than 30 days ago,” or “Within the last 30 days.” As a therapist, I would note a difference between suicidal ideation six months ago versus more than 10 years ago, and I would want to know the specific nature of these thoughts rather than just a yes or no to the question. I also had to indicate my pharmacy address, which seemed unusual because I was not seeking medication management.”
Occupational therapy: Telehealth platforms like Neofect and BlueJay Engage enable occupational therapists to provide remote care for patients with neurological or musculoskeletal disorders. These platforms use AI to develop tailored rehabilitation programs and monitor patients’ progress.
Nutrition and dietetics: AI-powered telehealth applications like NutriAdmin and Healthie allow dietitians and nutritionists to conduct remote consultations, track patients’ progress, and provide personalised meal plans—NutriAdmin uses a ChatGPT API to generate recipes—and recommendations.
Audiology: Tele-audiology platforms like SHOEBOX Audiometry and HearX Group offer remote hearing tests and consultations, enabling audiologists to assess and treat patients from a distance. AI algorithms can help analyse test results and recommend appropriate interventions.
Allied health patient education
AI can be a valuable tool for AHPs in supporting patient education by providing personalised, accessible, and engaging learning experiences. Health Tap, Ada Health, and Buoy Health are just three examples from an expansive and growing array of platforms.
Personalised education materials: AI-driven platforms can analyse patients’ medical data, preferences, and learning styles to provide tailored educational content that addresses their unique needs and concerns, intended to help improve patient understanding and adherence to care plans.
AI-driven gamification can potentially provide interactive learning experiences for patients and clients, making complex health concepts more accessible and (possibly) enjoyable. This can help improve patients’ health literacy and, more importantly, improve uptake and adherence to treatment plans.
Conversely, AHPs can use AI-based assessment tools to evaluate patients’ health literacy levels, identifying gaps in their understanding and helping allied health professionals target their education efforts more effectively.
With generative AI becoming ubiquitous in the creative industries, there are obvious applications for learning materials to be deployed by AHPs—generative AI can be deployed to generate and curate multimedia educational content, such as videos, animations, and infographics, catering to different learning preferences to make health information more engaging and accessible.
Virtual health coaches: As mentioned previously in this article, ’emotion AI’-driven virtual health coaches and chatbots are becoming widespread in providing patients with on-demand information and guidance, answering questions and offering evidence-based advice on various health topics. This could supplement traditional patient education efforts and enhance patient engagement.
Health monitoring and feedback: AI-enabled wearable devices and remote monitoring systems track patients’ health parameters and provide real-time feedback on their progress, educating patients about the impact of their lifestyle choices and the effectiveness of their treatment plans, promoting informed decision-making and self-management.
Support groups and online communities: AI can help facilitate and moderate online support groups and communities where patients can share experiences, ask questions, and learn from others with similar conditions. This can provide valuable peer support and enhance patients’ understanding of their health issues.
Support for interprofessional collaboration and communication
The broadening of AI integration into productivity and messaging platforms by Slack, Microsoft, Zoom, and Clickup has implications for the way healthcare teams collaborate.
It all depends on how the AI technologies are developed, but such integrations have the potential to better co-ordinate patient or client care by enhancing the efficiency and quality of collaboration across allied health disciplines and provide centralised decision support.
These integrations can potentially generate clinical draft summaries, combining data from sources such as electronic health records, images, lab systems, medical devices and claims systems, allowing clinics and organisations to standardise and access them in the same place.
Additionally, AI-driven chatbots like Copilot could assist allied health teams in retrieving pertinent data, clinical guidelines, and recommended practices, and propose appropriate actions or interventions tailored to individual patient conditions and preferences. Such AI chatbots can update records through natural language processing, streamlining communication and administrative tasks.
HCA Healthcare is currently trialling a system designed to extract key details from doctor-patient interactions to aid in the creation of medical notes. Healthcare providers utilise hands-free devices equipped with an app developed by Augmedix, which securely generates preliminary clinical notes automatically following each patient consultation.
AI-enhanced productivity and messaging platforms could also be augmented with predictive analytics tools—identifying patterns and correlations in patient data—and clinical decision support systems (CDSS) that provide consistent, evidence-based recommendations for diagnosis and treatment. Such tools and systems could help allied health teams proactively collaborate to develop targeted care plans and prevent miscommunications and discrepancies in patient care.
While AI can significantly enhance collaboration among allied health teams, it is crucial to remember the importance of human input and oversight. AI tools should be used to complement, not replace, the expertise of healthcare professionals, and ethical considerations should be prioritised to ensure responsible implementation.
Allied health training and education
Compared to some of the examples provided above, artificial intelligence in education (AIED) for health professionals seems to be quite nascent; frankly it’s difficult to find a blog article on the topic that hasn’t been generated using ChatGPT, with one or two exceptions.
Speculatively, AI could play a significant role in the education and training of allied health professionals—supported, but of course, by virtual assistants and chatbots—by offering innovative learning methods, personalised content, and enhanced assessment capabilities.
AI-driven adaptive learning platforms could customise educational content based on individual learners’ needs, strengths, and weaknesses. By analysing performance data, such systems could identify areas for improvement and adjust the learning materials accordingly, enhancing the effectiveness of the training process.
AI could be used to provide budding AHPs with a more lively technologically enhanced learning (TEL) experience. AI-powered virtual reality (VR) and augmented reality (AR) simulations could provide immersive, realistic training experiences for allied health professionals. Such environments allow learners to practice their skills in a controlled, risk-free setting, improving their competence and confidence in real-life scenarios.
Generative AI could provide realistic and complex case-base learning scenarios. Such an approach has the potential to enhance critical thinking and decision-making skills by exposing learners to various clinical situations and encouraging them to apply their knowledge in practical contexts.
Learning pathways could be strengthened by AI-driven assessment tools that provide instant, objective feedback on learners’ performance, identifying areas for improvement and reinforcing learning outcomes.
AI could facilitate collaboration among learners by integrating with platforms that enable knowledge sharing, peer review, and group problem-solving. This can help allied health professionals develop teamwork skills and benefit from the expertise of their peers.
AI-driven learning platforms could offer personalised continuing professional development (CPD) recommendations and resources, helping allied health professionals stay up-to-date with the latest research, innovations, and best practices in their fields.
Allied health research and development
Allied health professionals can use AI in research to streamline data collection and analysis, generate new insights, and improve the overall research process. Here are some ways AI can be used to assist allied health research.
Data mining and analysis: AI algorithms are capable of analysing large datasets quickly and efficiently, identifying patterns, correlations, and trends that may not be easily detected by human researchers. This can lead to new discoveries and hypotheses, informing the development of novel interventions and treatments.
Predictive modelling: AI-driven predictive models can help researchers forecast health outcomes, evaluate the effectiveness of interventions, and identify factors that contribute to specific health conditions. These models can improve the design and targeting of healthcare services and inform policy development.
Natural language processing (NLP): NLP techniques can be used to analyse text-based data, such as electronic health records, research articles, and social media posts, enabling researchers to extract valuable insights and identify trends in patient experiences, treatment approaches, and health outcomes.
Image and signal analysis: AI algorithms can analyse medical images, such as X-rays, MRIs, and ultrasound scans, as well as physiological signals like heart rate and blood pressure, with high precision and speed. This can help researchers identify markers of disease, evaluate the effectiveness of interventions, and develop new diagnostic tools.
Study design and participant selection: AI can help design more efficient and targeted research studies by identifying suitable participants based on specific criteria, predicting potential drop-out rates, and optimising study protocols.
Literature review and synthesis: AI-driven tools like meta-analyses and systematic reviews can help researchers efficiently identify, appraise, and synthesise existing evidence on a given topic, supporting the development of evidence-based practice guidelines and informing future research directions.
Conclusion
Share your experiences with the use of AI on The Allied Health Academy, or for contemporary updates on allied health, follow us on LinkedIn and subscribe to our Allied Health Insights newsletter.