
Allied Health Telehealth Triage To Manage Elective Surgery Waiting Lists
COVID-19 saw a rapid expansion in the uptake of telehealth services, including a range of innovations in allied health. However, one of the major legacies of COVID-19 was the disruption to normal hospital and primary health care treatment, delaying several services, including diagnosis and treatment. Substantial funding was injected into health services to support permanent telehealth, allowing GPs, specialists, and allied health professionals to consult with patients by phone or video call. This article looks at how allied health professions can use telehealth triage as a way to manage elective surgery waiting lists.
Growth in surgical waiting times
Between 2019 to 2021, COVID-19 caused the cancellation of elective surgery in many hospitals so that staffing and facilities could be re-deployed to effectively manage COVID-19. Workforce shortages continue to create large backlogs and delays in many areas of healthcare, including (but not restricted to) surgical waiting lists.
For most areas of surgery, the proportion of patients in Australia waiting for more than 365 days at least doubled over this period, as the list below illustrates:
- Otolaryngology, head and neck surgery: 7.6% to 17.4%
- General surgery: 1.8% to 4.5%
- Gynaecology surgery: 1.4% to 4.8%
- Neurosurgery: 1.7% to 5.4%
- Ophthalmology surgery: 4.6% to 12.7%
- Orthopaedic surgery: 5.0% to 14.5%
- Plastic and reconstructive surgery: 2.6% to 4.5%
- Urological surgery: 0.7% to 2.0%
- Vascular surgery: 1.2% to 4.1%
- Paediatric surgery: 1.6% to 5.2%
The consequences of long waiting times for surgery include the burden of disability on those unable to access treatment. When treatment is delayed, patients may deteriorate further, and lose condition, which means that the patient may need even greater intervention and take longer to recover from surgery.
Allied health professionals’ role in triaging surgical waiting lists

Triage is a process of prioritising needs and allocating care within the resources available.
Introducing allied health professionals into surgical triaging systems can reduce waiting lists; increase the appropriateness of referrals to interventions like surgery; seems to have few risks to patients and may even lead to better outcomes (this paper has a good summary of some relevant literature).
Allied health professionals can contribute to triaging surgical waiting lists to determine whether (a) patients should be referred for surgery (should stay on the surgical waiting list) or (b) should be referred to other services as an alternative to surgery or (c) whether receiving other services while they are on the waiting list might improve their symptoms and reduce their need for surgery or improve their surgical outcomes.
The number of patients waiting more than twelve months for orthopaedic surgery has nearly tripled since 2019. Orthopaedics provides a good example of the use of allied health triage of waiting lists. For example, one study found that triaging patients with lower back pain through an advanced practice physiotherapy clinic prior to review by orthopaedic specialist reduced waiting times and resulted in up to 71% of patients being removed from orthopaedic surgical wait list. Another study involved triage of patients on an orthopaedic waiting list for foot surgery. The podiatrist identified patients on the waiting list who were potentially suitable for conservative management are were provided with non-surgical podiatry interventions and discharged if appropriate. Those who still required surgical intervention after receiving the interim conservative treatment by the podiatrist resumed their previous place on the orthopaedic waiting list. The intervention reduced waiting times for patients on the surgical list and improved patient flow.
Podiatrists are used effectively in orthopaedic departments to manage foot and ankle pain, a common problem affecting one-quarter of adults aged 45 or over. Other allied health professionals such as physiotherapists triage patients with hip, knee and back complaints. Psychologists play an essential role in treating mental health problems associated with chronic pain. Interdisciplinary clinics, where allied health staff work closely with surgeons and other medical professionals, are becoming critical. Unfortunately, funding is not always available to run these clinics inside the hospital. This is where telehealth fits in.
Allied health telehealth triage
There are increasingly innovative approaches that allow allied health professionals to interact virtually or asynchronously with patients to help manage waiting lists. Not all of the examples below are derived from allied health literature, however there is the potential to offer allied health services by modifying the approaches used below to appropriate settings.
Asynchronous review of medical records, such as diagnostic imaging
Tele-orthopaedic services using asynchronous methods to review radiographs without direct patient involvement. These models have largely been used in fracture clinics, but may be valuable to aid decision making for orthopaedic triage
Telephone triage of surgical waiting lists with the option of referral into other services
Physiotherapists using telehealth triage with a structured assessment tool of patients on an orthopaedic waiting list, providing a range of alternative interventions for appropriate patients.
Coaching, counseling, support and education
Allied health practitioners play a vital role in educating patients on the realities of surgery—recovery times, risks and potential complications. Such education empowers patients to manage their expectations.
Remote monitoring of vital signs
Again, while not specific to allied health, the use of remote monitoring of patients using m-health to determine changes or deterioration in health status may help identify those most at risk and in need of alternative interventions. This study used m-health to monitor patients awaiting cardiac surgery, with promising results.
Better preparing patients for surgery or alternatives
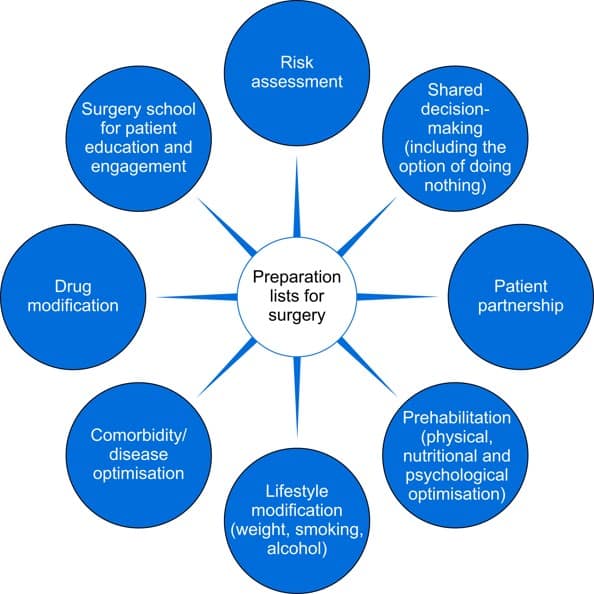
This recent paper suggests that waiting lists should be called “preparation lists” and provides a range of potential activities that can be implemented while patients are awaiting surgery to help improve their outcomes., summarised in the diagram below. Again, these interventions are not specific to allied health, however pharmacists, dietitians, lifestyle coaches, psychologists, exercise physiologists, physiotherapists, and other multidisciplinary team members could all play a role in the optimisation of patient outcomes using most of the interventions below through telehealth access.
With long waiting lists for many services, there is an imperative, and indeed even an ethical obligation to minimise the burden of disease and the risks of declining outcomes for patients as a result of long waiting times for services. The options listed above require some creative thinking as well as some service redesign, however there are a number of opportunities to increase the independence and mobility of patients awaiting surgical interventions.
Find out more about Telehealth
Here are some links to websites and resources for AH practitioners interested in telehealth:





