Podiatry – The A To Z Of Allied Health
We tend to pay little attention to our feet, until the point that they become painful or cause problems. Foot problems are indeed very common, with approximately 3% of all GP encounters related to foot or ankle pain. It is likely that most people will experience pain or other problems with their feet over their lifespan. Podiatry, also known as chiropody in some countries, is the allied health profession involved in the treatment of people with foot and lower limb conditions.
What do podiatrists do?
Podiatrists use their refined clinical skills and numerous modalities to conduct thorough assessments, and diagnose and manage a range of acute and longer-term foot health conditions, as well as the lower extremities in some countries.
Some of the more common reasons people seek podiatry care include:
- Skin conditions affecting the feet such as callous, corns, warts, and fungal infections such as athlete’s foot
- Nail problems such as ingrown toenails or fungal nail infections
- Foot pain due to injury or arthritis
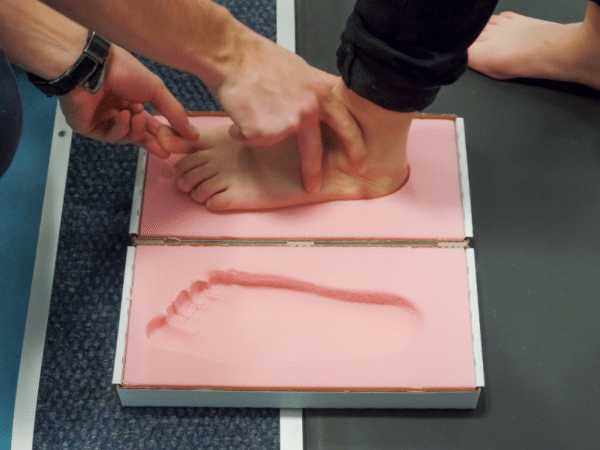
- Foot deformity or a biomechanical problem that requires special devices called orthotics (or orthoses) and/or accommodative footwear
- Chronic wounds due to diabetes , and/or problems with circulation, injury and/or infection
- Numbness or other neurological symptoms
- Paediatric issues such as children who walk on their toes or experience developmental delay
Podiatrists play an important role in preventing and managing foot health problems due to chronic health conditions such as diabetes, cardiovascular disease, neurological conditions, autoimmune conditions, and others. They regularly conduct thorough assessments, to identify a person’s risk of serious foot problems and develop a management plan accordingly.
A podiatry consultation typically involves the podiatrist gathering information about a person’s medical and foot health history and a physical examination of the lower limb. Clinical assessments may incorporate equipment such as blood pressure cuffs and dopplers to measure and assess circulation, and devices to investigate nerve function. Podiatrists may also refer for imaging (e.g., X-ray or ultrasound) to aid their clinical and diagnostic reasoning process. Depending on the issue and diagnosis, podiatrists use various medical-grade instruments to treat any issues they may come across, such as nail clippers, files and scalpels. They may prescribe orthotics, and almost always provide foot health and footwear education.
Podiatrists also conduct biomechanical examinations and gait assessments to observe how the feet and lower limb function during everyday movement. In recent years, technology has been developed to support 3D gait analysis.
Podiatrists may work with children who have symptoms related to a health or developmental condition or may have one or more of the problems described above. Although all podiatrists are qualified to work with children, paediatric podiatry practice is becoming increasingly specialised, as more research emerges about the foot health needs of children.
Podiatrists may also work with athletes and sport clubs to provide specialised foot health advice to prevent and manage injuries. They also work with older people to improve and maintain their function and mobility and to reduce the risk of falls.
In the USA and Canada, podiatrists are medically trained and have a wider scope of practice, akin to that of a medical physician. In Australia and the UK, podiatrists can undertake additional study and/or supervised practice to become an endorsed podiatry prescriber. Endorsed podiatry prescribers can prescribe a limited range of medicines to treat foot health conditions. The most commonly prescribed medicines by endorsed podiatrists include anaesthetics, antifungals, antibiotics, and pain medications. Podiatrists in the US are trained surgeons, managing surgical care of deformities and fractures. Not all podiatrists will choose to perform surgical procedures, however they are able to undertake a range of interventions from smaller in-office soft-tissue procedures through to reconstructive rearfoot surgery.
In Australia and the UK, some podiatrists undertake additional training to become a qualified podiatric surgeon.
Where do podiatrists work?
Podiatrists work in many countries including Australia, New Zealand, the UK, Canada, the USA, Hong Kong, Singapore, and India.
Podiatrists are key members of multidisciplinary healthcare teams in hospital, outpatient, and community-based health services. In Australia, most podiatrists (up to 80%) work in private practice. In the UK there is more of an even split of podiatrists working for the National Health Service and fewer working in private practice.
Some podiatrists work in various hospital or clinical settings, and others in solo private practice settings. Podiatrists deliver important services to people living in residential aged care facilities who may be at risk of foot health issues including chronic wounds (ulcers) or may have trouble managing their own foot health care. Some work in higher education and research institutions.
Important character traits of podiatrists
Podiatrists often need to develop evidence-based strategies to effectively manage routine, challenging and complicated foot related issues so excellent problem-solving skills are a must. They also need to have good dexterity to perform their job adequately.
Podiatrists may spend up to one hour with clients and often see them on an ongoing basis, so they tend to develop a good rapport. Clients may divulge information to their podiatrist, rather than other healthcare professionals with whom they spend less time, so podiatrists must be good listeners, sensitive, compassionate, and communicate effectively.
Podiatrists are very busy allied health professionals, often working to a tight schedule, so good time management skills are a must.
What are the professional education and regulatory frameworks for podiatrists?
Currently in Australia, New Zealand, and the UK, podiatrists are required to complete a bachelor’s degree in podiatry which usually takes between three and four years to obtain. Aspiring podiatrists undertake clinical practice as part of their educational preparation. In the UK, there are also some apprenticeship-style pathways to becoming a podiatrist.
In the US, podiatrists complete similar training to physicians; that is, four years’ podiatric medical school education followed by three years of mandatory hospital residency training. They may then go on to complete fellowship training.
In some countries, such as Singapore and Hong Kong, where podiatrists practice and are recognised as key members of healthcare teams, there are no local training schools for podiatrists and these allied health professionals attain their qualifications overseas.
Regulatory frameworks
Podiatrists are regulated nationally in several countries including the UK (Health and Care Professions Council), Australia (Australian Health Practitioner Regulation Agency), and New Zealand (Podiatrists Board). In Hong Kong, podiatry is regulated via the Hospital Authority. In Canada and the USA, podiatry is a regulated profession, however the licencing and regulation varies across states. In the US, podiatrists are considered physicians and surgeons rather than allied health professionals. In Singapore, podiatry is not one of the allied health professions regulated by the Allied Health Professions Council.
Workforce considerations for podiatrists
Widespread workforce shortages are felt by the podiatry community, with concerns about the reduction in intakes of podiatry students, as well as the retention of qualified podiatrists. In the UK, Health Education England is working to develop solutions to this problem, including alternative training pathways. In Australia, the podiatry workforce recruitment problem is complicated by the fact that podiatrists are predominantly employed in the private sector. This means that critical workplace learning opportunities for podiatry students are limited and this has implications for the training pipeline.
Prescribing rights
Advances in the scope of podiatry practice in the UK and Australia have been made over the last two decades, specifically in terms of the right to prescribe scheduled medicines. Although legislative changes have meant that endorsed Australian and British podiatry prescribers can independently prescribe a restricted list of medicines and some podiatrists also have local anaesthetic accreditation, legislative barriers to podiatry prescribing remain and the full benefits of these advances to podiatry practice have not been realised.
In the UK, Matthew Fitzpatrick and Alan Borthwick describe a similar albeit more complicated story for podiatrist prescribers. Separate but interrelated regulations governing the prescription of scheduled drugs: the Human Medicines Regulation (2012) and Misuse of Drugs Regulations (2001), have been amended at different times and in different ways over the decade since podiatrists were initially granted independent prescribing rights in the UK. These amendments have resulted in differences in the two regulations leading to reclassification of several drugs, and the need for the Royal College of Podiatry to make further submissions to the Commission of Human Medicines and other bodies, to remedy the discrepancies in the relevant regulations and legislations.
Find out more about podiatrists
Here are some links to websites and resources for and about podiatrists:
- Australian Podiatry Association
- The British Chiropody and Podiatry Association
- Royal College of Podiatry
- American Podiatric Medical Association
- Canadian Podiatric Medical Association
- Podiatry New Zealand
- Podiatry Association – Singapore
- Hong Kong Podiatrists Association
- The Institute of Chiropodists & Podiatrists
- The SMAE Institute
If you have questions about the podiatry profession, or if you wish to share your experiences as a podiatrist, please leave a comment below.
Subscribe to Allied Health Insights to receive incisive and up-to-date allied health solutions and commentary. | Browse our professional career insights into the allied health professions here.
If you offer professional development or business support services for podiatrists or their employers, please list your business on our Service Directory.
AHP Workforce provides allied health workforce planning, strategy and consulting for employers, managers and public sector stakeholders. For allied health workforce solutions, contact us today.